|
The colon is the part of the large intestine that connects the small intestine with the rectum and anus. Together, they form the final part of the digestive system, responsible for absorbing water, minerals, nutrients, and shaping stool. Colorectal cancer encompasses all tumours that can affect the first part of the large intestine up to the rectum and/or anus. Dietary priorities during the treatment of colorectal cancer are to ensure adequate nutritional status, improve symptoms, and avoid complications. However, it can be complicated to establish a general diet for this disease, as it depends on several factors: where the tumour is located, the treatments and therapeutic options used, and the patient’s nutritional status and social environment, amongst other factors. |
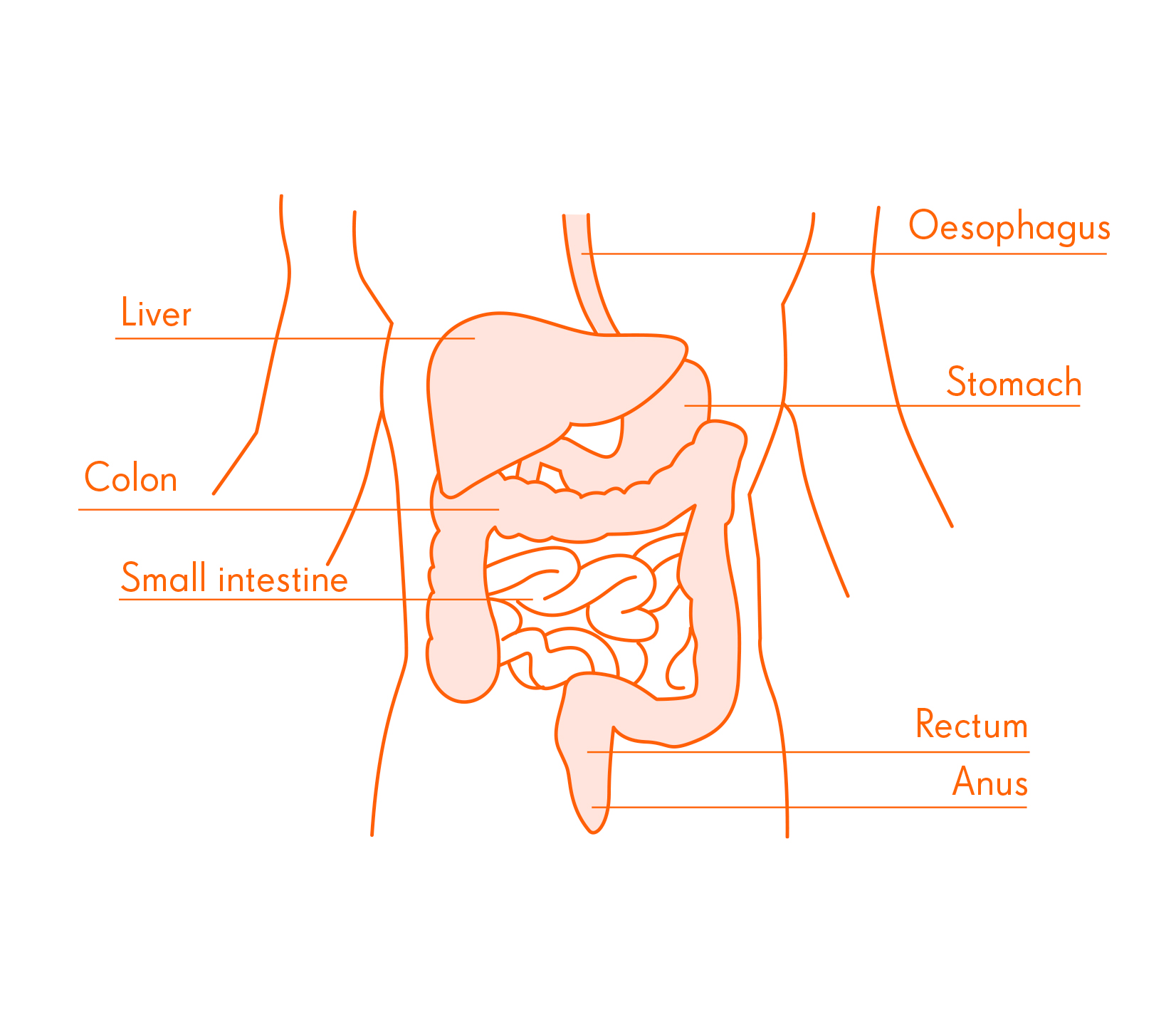 |
Treatment may cause effects that require some restriction in the diet or, contrarily, may not involve any dietary restrictions: there may be a risk of bowel obstruction (occlusion) or the placement of a bag to collect stool (ostomy). In general, to ensure an adequate nutritional status, in addition to following the “General recommendations on nutrition during cancer treatment”, in colorectal cancer it is important to:
- Pay special attention to the fibre in food and adjust your intake according to your situation. Fibre is a part of whole-food and plant-based foods (fruit, vegetables, pulses, nuts, dried fruit and whole grains) that the body cannot digest, and reaches the large intestine to be broken down by the micro-organisms that live there. The consumption of fibre should be adjusted in situations such as:
- When the tumour occupies an important part of the intestinal passage, where a high intake of fibre could cause abdominal pain or aggravation.
- When there is a risk of bowel obstruction.
- When a patient has had an ostomy (ileostomy or colostomy) as a result of a surgical procedure. This consists of an artificial opening in the small intestine or colon into the abdomen and outside the body to allow bodily waste to pass through. The opening is called an ostomy and is where a special bag, attached to the skin, is placed to collect stool. This placement may be temporary or permanent.
- When diarrhoea occurs.
In any of these situations, it will always be the specialist who will indicate the degree of fibre restriction. In case of persistent constipation or severe abdominal pain, consult the specialist.
- Recognise the behaviour of foods. In addition to fibre, during colon cancer treatment it is important to be aware of the effect that different food groups have on digestion, bowel movements and stool. It is a good idea to write a food diary during the first few weeks.
- Check for any food-drug interactions. In this type of cancer, possible interactions have been described with plants and herbs, such as hypericum and aloe; foods such as grapefruit and grapefruit juice; and with nutrients in certain foods and supplements, such as folic acid. These interactions may occur depending on the treatment prescribed, so always consult the oncologist.
- Adapt the diet according to side effects and other symptoms that may appear, based on the dietary-culinary recommendations set out below.