|
Head and neck cancer includes all tumours affecting the face area and the neck. There are different types of head and neck cancers, which, depending on the exact location of the tumour and the treatment received, will have different side effects. The main recommendation during treatment is to eat, which is essential to maintain energy and better tolerate the medication. In general, eating sufficiently is not usually a problem, but it can be a challenge during treatment for head and neck cancer. |
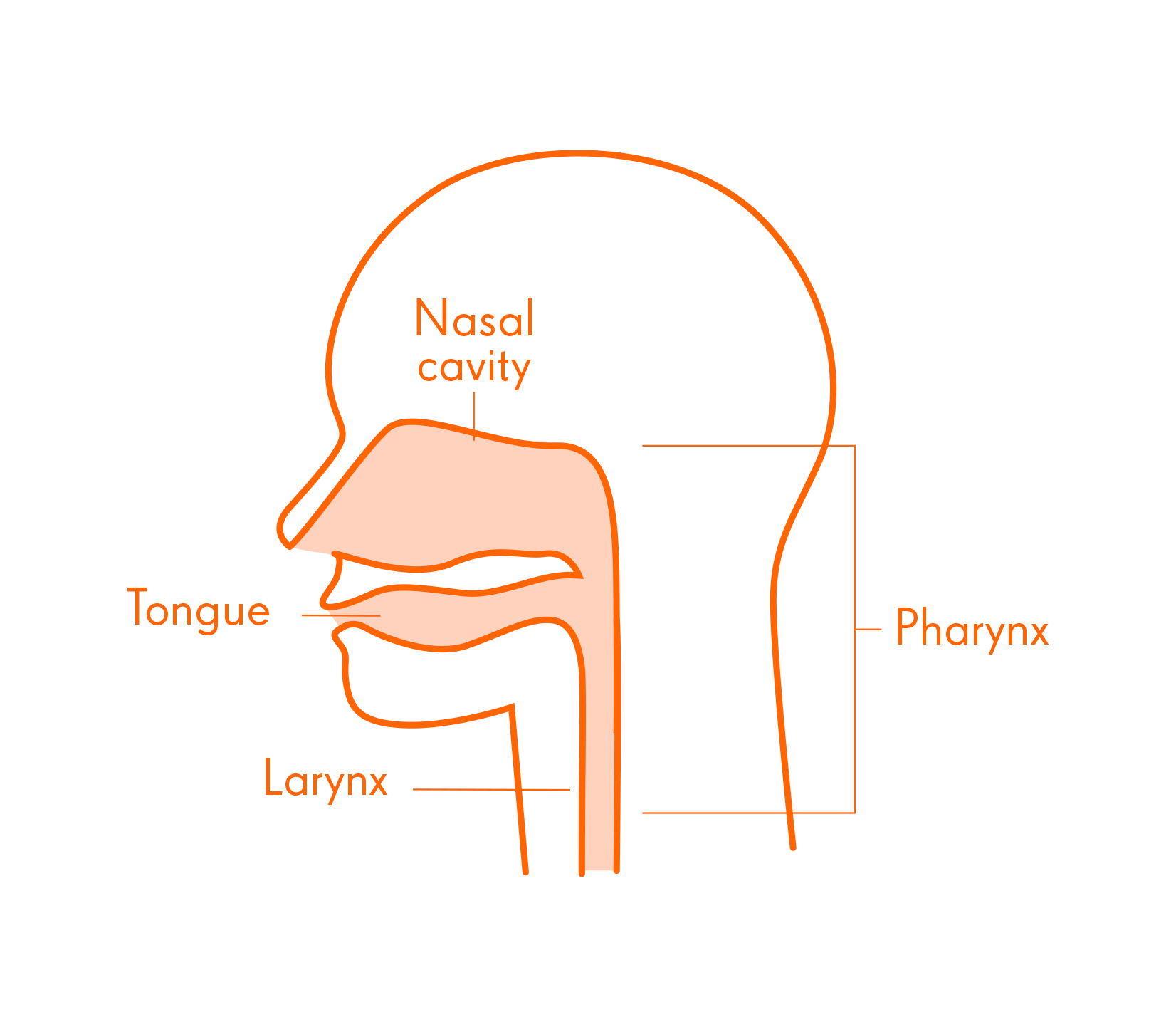 |
Affected individuals, due to the location of the tumour or the treatment received, may suffer difficulties with chewing or swallowing. This can lead to complications in ingesting food. Head and neck cancer is one of the tumours which causes the highest frequency of malnutrition. In case of inability to eat or significant weight loss, seek nutritional support from your oncologist.
In addition to following the “General recommendations on nutrition during cancer treatment”, in head and neck cancer, the following guidelines should also be followed:
- Divide food intake into several meals a day. Due to the difficulty involved in eating or drinking, increase the number of meals (breakfast, mid-morning snack, lunch, afternoon snack, dinner, and supper) in order to cover the nutritional needs throughout the day.
- Adapt the texture of food. During the treatment of head and neck cancer, discomfort, pain and difficulty in drinking and eating (pain and/or difficulty in swallowing and sores in the mouth and/or throat) are very common. In order to avoid decreased intake of food, modifying the texture of food or the viscosity of liquids can alleviate discomfort and pain, and facilitate chewing and swallowing. The texture should be adapted according to the needs of each situation: simple considerations and modifications may be sufficient, or it may be necessary to completely blend or mash all preparations and avoid different textures. For this reason, it is always necessary to assess which adaptation is the most appropriate, following the indications of the oncologist and registered dietitian in charge.
- Check for food-drug interactions. Possible interactions have been described with plants and herbs such as hypericum and aloe, foods such as grapefruit and grapefruit juice, and alcoholic beverages. These interactions could occur depending on the prescribed treatment, so always consult your oncologist on a case-by-case basis.
- Adapt your diet to the possible side effects or symptoms derived from treatment based on the dietary-culinary recommendations set out below.